The “caring for the mental health of the medical workforce report” describes the quantitative results of a survey of doctors and medical students in October 2018. The participants were self-selecting, but over 4,300 people responded, including 1,400 medical students.
The survey used the Oldenburg Burnout Inventory and 80% of respondents had scores that correlate with high, or very high, risk of burnout. Burnout is now an internationally recognised and defined syndrome in the ICD 11.
“Burn-out is a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by three dimensions: 1) feelings of energy depletion or exhaustion; 2) increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job; and 3) reduced professional efficacy. Burn-out refers specifically to phenomena in the occupational context and should not be applied to describe experiences in other areas of life.”(1)
However, the clinical cut off for when someone is considered “burnt-out” remains a contentious issue, as the research inventories were not designed as diagnostic tools.
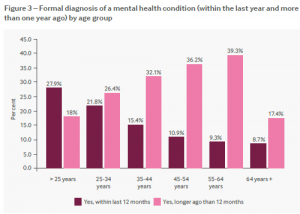
The results of the BMA survey reflect the findings in the general population collected in Adult Psychiatric Morbidity Survey (APMS) 2014, which showed a fifth of men (19.5%) and a third of women (33.7%) have had mental health diagnoses confirmed by professionals. The APMS also found a noticeable increase in the prevalence of common mental health problems for both men and women between the ages of 55 and 64. (2)
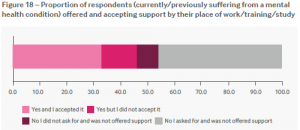
The figure below shows that a large proportion of people surveyed with mental health diagnoses asked for support at work and were not offered it. This again highlights the need for better occupational health services in our organisations with relevant staff trained in support procedures for staff and students with mental distress.
The findings detailed in this BMA report add to the body of work published this year describing the mental wellbeing of doctors:
NHS Staff and Learners Mental Wellbeing Commission. Health Education England.
Health Education England suggest a need for self-referral access and rapid access referral pathways, through priority requests from primary care or occupational health clinicians, to a practitioner psychological treatment service locally, or nationally.
The BMA say they will also be releasing a report on the qualitative data from the survey. In addition to this, look out for publications from the groups below later this year on Doctors’ wellbeing:
GMC review of the wellbeing and health of the medical profession
Access the full BMA report via the link below:
Caring for the mental health of the medical workforce. British Medical Association.
References:
- World Health Organisation. International Classification of Disease 11 for Mortality and Morbidity Statistics. Version 04/2019. QD85 Burn-out. Available from: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281 (Accessed 29/04/19).
- NHS Digital. National Centre Social Research and the Department of Health Sciences, University of Leicester. Adult Psychiatric Morbidity Survey (APMS). Mental Health and Wellbeing in England 2014. Available from: https://files.digital.nhs.uk/pdf/q/3/mental_health_and_wellbeing_in_england_full_report.pdf (Accessed: 29/04/2019).